Lytico-Bodig on Guam
Table of Contents
Share This
Long studied, now disappearing disease
Lytico-bodig is the local name for a complex of neurological diseases (or diseases that affect the nervous system) on Guam that resembles amyotrophic lateral sclerosis (ALS or Lou Gerhig’s disease), Parkinsonism-Dementia (PD) and possibly Alzheimer’s disease. Because of its occurrence in a relatively unique and isolated population, lytico-bodig has been widely studied by various groups of researchers in the hopes of finding its cause and possible cures.
Now known formally as ALS-PD complex of Guam (ALS-PDC), its prevalence in the 1950s and 1960s brought a sense of immediacy to working on Guam as patients passed away from the disease. The major research efforts sought to answer the question of whether lytico-bodig is a genetic or hereditary disease, or one caused by some environmental factor or factors? Although numerous theories were brought forward, there is still no definitive set of causes or cures. With advances in medical technology, strides have been made toward understanding lytico-bodig clinically, however, only few have studied its social or cultural impact on the CHamoru/Chamorro people. Although reports of neurological disease resembling lytico-bodig among the Chamorros occurred as far back as the early 1800s, formal study of the disease would not take place until more than a century later.
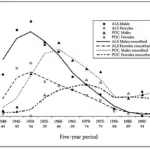
At its peak in the 1950s, lytico-bodig became the leading cause of death for Chamorros, affecting some 420 per 100,000 Chamorros, at a ratio of 2:1 males to females. ALS was seen more in Chamorros, while PD was seen in both Chamorro and Filipino natives. According to Chris Plato, et al., the incidence of ALS peaked from 1950-1954 in both males and females, but by the late 1950s, the incidence of ALS began to decline. Also, the incidence of PDC in males peaked from 1960 to 1964, and then declined steadily until 1980. The incidence of PDC in females peaked in 1970 to 1974, then rapidly declined in the early 1980s. Ralph Garruto and Richard Yanagihara reported that from 1950 to 1979, the age of onset ranged from 20 years to 72 years old, and increased for both men and women by three to four years. Today, however, lytico-bodig, is extremely rare.
The increase in cases of lytico-bodig after World War II caught the attention of scientists who were also looking at other neurodegenerative diseases. Work was being done in Papua New Guinea on a disease called kuru which affected the Fore people. ALS and PD in the form of lytico-bodig was seen in Guam but a similar occurrence of ALS and PD was reported in five villages in the Kii Peninsula in Japan. According to Garruto and Yanagihara, all these places presented a unique site for research as a “natural experimental model of disease” because of their relative isolation, their concentration of patients with the disease, and unique ecological factors. In addition, they were seen as ideal for studying the global impact of neurodegenerative diseases in ways that would not have been possible with a larger, mixed population. While the causes of kuru were uncovered by the 1980s, the pathogenesis, or causes and development, of lytico-bodig have not been definitively revealed.
Symptoms
Lytico-Bodig is a neurodegenerative disease. Neurodegeneration is an umbrella term for any condition that results in the progressive loss in the structure or function of the neurons or nerve cells. Diseases like ALS, PD and Alzheimer’s affect nerve cells in the brain. Although lytico-bodig are worded together, they actually represent two different diseases. The term “lytico” comes from the Spanish word paralytico which means weakness. “Bodig” comes from the Spanish word bodega, or warehouse. Medical anthropologist Verena Keck wrote that “bodig” came from the nickname of a man who owned a bodega in Saipan during the German colonial administration (1898-1917) who had symptoms of the disease when he returned to Guam. Lytico patients have ALS symptoms, while patients with bodig have symptoms that resemble PD. Some patients, however, may have symptoms of both.
ALS affects motor neurons, which are the nerve cells that control muscles. As the disease progresses, symptoms such as weakness, wasting and eventual paralysis of the legs and arms become apparent. Patients become unable to care for themselves and are usually bedridden, unable to speak and swallow. They also have difficulty breathing. The paralysis of the muscles that control breathing and swallowing is what eventually kills ALS patients. However, even though they are physically debilitated, ALS patients still have memory and are able to think clearly.
On the other hand, Parkinson’s disease is characterized by a slowness of voluntary motor function. Muscles become rigid, and tremors or uncontrolled shaking of the hands and legs also occur. Parkinson’s patients also exhibit a characteristic stooped posture as the disease progresses. Parkinsonism is usually accompanied by an early onset progressive dementia–a loss of cognitive abilities such as memory, language and behavior. Patients with dementia become forgetful, confused and irritable, and may even have hallucinations as the disease runs its course. Some researchers today believe the dementia that occurs with lytico-bodig is similar to Alzheimer’s disease, but this association is still unclear.
Vince Diego, a biological anthropologist at Texas Biomedical Research Institute (TBRI) in San Antonio, says there are two lines of thought on this issue: one is that the lytico-bodig has somehow morphed or changed into a disease that resembles Alzheimer’s, and another that finds lytico-bodig as a distinct neurological disease from Alzheimer’s. The degeneration of brain tissue in Alzheimer’s disease can be seen when examined after the patient has died. The damaged tissue, made up of dead or dying nerve cells, is called a lesion. Patients with lytico or bodig, may also show lesions in the brain, in particular, lesions known as neurofibrillary tangles (NFTs).
However, in the 1960s and 1970s, 70 percent of the Guamanians tested had NFTs in their brains, but without the clinical disease. This led researchers to ask if, perhaps the development of NFTs are a preliminary phase of the disease? In any case, this situation demonstrated the difficulty in identifying true controls for the disease on Guam. Another symptom which seems to be associated with ALS/PDC is linear retinal epitheliopathy, which is a disorder of the eye. The retinal epithelium is the pigmented layer of the retina at the back of the eye that anchors photoreceptors, or the cells that sense light and help with vision. There are no symptoms except for unusual tracks that appear in the retinal layer, but it seems to appear in half of Guamanian Chamorros with ALS and PDC and to precede the onset of the disease.
The onset of lytico-bodig is currently late in life, with symptoms appearing in the 60s or 70s, sometimes not until the 80s. Patients usually die within four to five years, but there have been cases where individuals died within months of diagnosis, and others survived more than 30 years. In the past 50 years the age of onset has increased and the number of cases of the disease has declined.
While lytico is no longer seen and bodig is rare, dementia still occurs among elderly Chamorros. In Guam, lytico-bodig seems to run in families, even among siblings. They might even represent the same disease but different endpoints. Both are late-onset (although there have been reports of individuals as young as fifteen years of age being diagnosed) and always fatal. Earlier studies showed that the sex ratio of the disease was 2:1 and even 3:1 at one point males to females; but by 1982, the ratio was even, at 1:1 males to females.
While the disease seemed to peak after World War II, especially in the southern region of Guam, it also showed a dramatic decline by the 1970s and 1980s. The large concentration of ALS and PD in Guam’s southern villages brought up many lines of inquiry regarding the causes lytico-bodig, including genetic or environmental factors, or a combination of genetics and environment.
Long search for the cause of Lytico-Bodig
Genetics
The exact cause of lytico-bodig has eluded researchers for decades. Neuroscientists believe, though, if they can figure out the cause, they may be able to figure out a cure for this and possibly other debilitating neurological diseases. Because the disease was observed to run in families, both generationally and among siblings, researchers believed the cause might be genetic.
In 1957 a case-control registry was developed to allow observation of first-degree relatives (parents, siblings and children) and spouses. The spouses served as the unrelated control group. The studies of these individuals showed that parents, siblings and spouses of patients had a significantly increased risk of developing the disease compared with the relatives of the spouses. Offspring of patients also did not have an increased risk, but this is probably because they were not old enough to develop symptoms at the time of the study. The unrelated spouses getting the disease supported the idea of a “household effect.” When offspring of patients reached the age of risk, they showed an increased risk of the disease compared with offspring of the non-related spouses (control).
Humåtak had the highest concentration of patients and a pedigree–a diagram, similar to a family tree, that shows the pattern of genetic inheritance (and by extension, diseases or other conditions) of a family–was produced for the village by Chris C. Plato. Plato also led the long-term studies of lytico-bodig in families on Guam. The pattern of clustering of families with disease was also observed in the Kii Peninsula of Japan.
However, despite numerous genetic studies of families on Guam, there was no firm evidence that genetics was a major factor in getting the disease, but rather, something in the environment. Studies of genetics have not revealed any kind of specific mutation for lytico-bodig. Also, the disease was rapidly disappearing–genetic disorders do not necessarily disappear in a generation. The rapid decline of the disease was believed to be associated with development, modernization and the introduction of new kinds of foods. Nevertheless, some neuroscientists continue to pursue the notion that certain individuals may have a genetic predisposition for the disease.
Metals
In 1961 a team of scientists looking at ALS in the Kii Peninsula of Japan found that the disease occurred in areas where river and drinking water were low in minerals. The team proposed a metal hypothesis whereby a possible mechanism for ALS was the involvement of metals like aluminum, manganese and calcium. Low environmental levels of calcium and high levels of aluminum were reported in Guam, Western New Guinea and the Kii Peninsula.
On Guam, the soil on the southern end of the island was composed largely of a shallow red clay called laterite (which, incidentally, was similar to the soil found in the Western New Guinea villages). In the 1970s and 1980s, various studies on Guam by teams led by Richard Yanigihara, D. Carleton Gadjusek, and Ralph Garruto and their colleagues looked at environmental metals and brain metabolism. It was reported that 37 percent of Guamanians with lytico-bodig showed disturbances in calcium and vitamin D metabolism. Aluminum in the nervous system was also reported in several patients on Guam with ALS and PD. Abnormal deposits of calcium, aluminum and silicon were also found in Guamanians who did not show the disease (“neurologically normal”) but that had NFTs; however, these deposits were not present in those who did not have NFTs.
The presence of these metals, in combination with the mineral calcium, may disrupt the normal function of the nerve cells and eventually lead to cell death. The scientists proposed that individuals with a predisposition, such as a defect in their metabolism, combined with the elevated levels of metals in the environment, and provoked by a period of nutritional deficiency of calcium and magnesium, may have lead to greater absorption of the metals in the neurons. Studies two decades later by MC Hermosura, et al., provided further evidence for this theory, but the exact process is still not known.
Cycads (fadang)
Probably the most well-known proposed cause of lytico-bodig involves neurotoxins in cycad seeds. In the 1960s, early researchers Leonard Kurland and Donald Mulder postulated that poisons in cycad seeds, ingested over time, possibly caused the disease on Guam. Unlike other Pacific islands, the Chamorros on Guam would leech the seeds of the false sago palm (Cycas micronesica, or fadang in Chamorro) to remove the poisons and then ground them into flour for baking.
The three main toxins released by the cycad are β-N-methylamino-L-alanine (BMAA), cycasin and steryl glucosides, and each one has been advocated by different scientists as the cause of lytico-bodig. Chamorros had been consuming fadang for more than 150 years, a practice introduced to them by Mexicans through the Spanish Acapulco-Manila Galleon Trade. However, research over the next decade did not provide any definite link between cycad toxins and ALS or PD.
In the 1980s, however, another team of researchers led by Peter Spencer, found that the toxin BMAA, when given to cynomolgus monkeys (Macaca fascicularis) in large amounts, caused the monkeys to develop changes in their motor neurons. The amount of BMAA in cycad fruit is about 1g/kg, so a monkey would have to be fed about 42 kg of unwashed cycad for about 12 weeks to produce a result. An adult human would have to consume about 17.5 kg of unwashed cycad a day, or about 1500 kg in 12 weeks to show the effects seen in the monkey. However, Chamorros process cycad before eating it by washing it thoroughly over several days so only a trace amount is left.
Although Spencer acknowledged that BMAA was probably not the cause of ALS/PD on Guam, he believed there may have been some other yet undiscovered toxin that was responsible. In the early 2000s, the cycad toxin theory was brought up again with Paul Cox and Oliver Sacks who observed a decline in lytico-bodig that paralleled a decline in the fruit bat population on Guam. They proposed that while cycad processed into flour was not toxic enough to produce lytico-bodig, there may be other elements in the Chamorro diet that could magnify the effects of the neurotoxin. Eating fruit bat (Pteropus mariannus mariannus, or fanihi in Chamorro), for example, a local delicacy, might contribute to the possibility of the disease. The scientists suggested that fruit bats that eat the cycad accumulate the toxins in their tissues but may not themselves be affected by the toxins.
However, if people ate enough of the fruit bats over the course of their lifetime (perhaps beginning in childhood), the toxins could accumulate in their bodies and eventually cause the disease. Cox also suggested that the presence of cyanobacteria in cycads which could produce BMAA naturally, may also be considered a possible cause. Cox and his colleagues also reported that BMAA was found in ALS and PD patients on Guam.
There are several reason for discounting the cycad as the cause of lytico-bodig. First, there are no examples of a natural neurotoxin causing disease decades after exposure. Second, the curve for the decline in fruit bats (which are almost extinct) does not align with the decline in cases of lytico-bodig on Guam. Additionally, Cox’s findings of naturally-producing BMAA cyanobacteria and BMAA in ALS and PD patients on Guam could not be reproduced. Furthermore, in the other two places exhibiting similar conditions to lytico-bodig–the Kii Peninsula and Western New Guinea– only the Auyu of Western New Guinea ate fruit bats, and it was not known if the fruit bats ate cycad.
It was noticed by Gadjusek’s team that with economic development and the introduction of new kinds of foods, there was a decline in the disease. This seems to better support the metal hypothesis and the idea that a rapid environmental change seemed to cause the ALS and PD.
Gene-Environment interaction
By the 1990s, a new approach to understanding the interaction of genes and the environment as a possible cause for lytico-bodig was pursued using advances in molecular genetics and DNA technology. With 40 years of observation and data collection, it seemed more likely that a combination of genetic and environmental factors increased the risk of getting ALS or PD. One line of inquiry involved looking for genetic mutations in the mitochondrial DNA of Guam ALS and PD patients that affected levels of metal and calcium that could impact nerve cells. Later studies in the 2000s reported genetic mutations in nuclear DNA that affected calcium absorption in nerve cells that could lead to cell death.
These mutations in both nuclear and mitochondrial DNA, coupled with the environmental conditions of the island, are being used to support the theory of a gene-environment interaction for ALS and PD on Guam. The gene-environment interaction theory provides a mechanism for metals linked to lytico-bodig to enter and accumulate in patients.
Protein transformation
In the 1950s, Gajdusek studied kuru, a disease that affected the Fore people of Central New Guinea. He demonstrated that kuru was passed on through a prion, a kind of “mis-folded protein,” that was ingested through a cannibalistic ritual. When brain tissue of infected patients was injected into monkeys, the monkeys developed the disease. Gajdusek tried to see if ALS, PD and Alzheimer’s also could possibly be transmitted in a similar way, but he was not able to demonstrate this.
However, in 2008, research involving stem cells (cells in the human body that can potentially develop into different cell types) showed that healthy stem cells injected into patients with Parkinson’s disease were transformed and would accumulate the same mis-folded proteins that caused Parkinson’s. Similar experiments with other neurodegenerative diseases were conducted and showed similar transformations, which may suggest that the disease progresses slowly from cell to cell throughout the nervous system.
Although it is not known what could cause the mis-folded proteins to form, they do seem to occur after certain kinds of acute infections, such as post-encephalatic parkinsonism (PEP), which occurs after encephalitis lethargica. Another disease, subacute sclerosing panencephalitis (SSPE) occurs after measles infection. These diseases show no symptoms for a long time after exposure, have a long incubation period, and then show a slow decline.
There has been some speculation that the 1918 influenza epidemic, which killed 858 people in two months, may have some connection to lytico-bodig patients, most of whom were born before 1920. However, there is no hard evidence to support this.
John C. Steele, a neurologist who has worked on Guam and researched lytico-bodig for decades believed that Guam holds the key to understanding the disease. While lytico-bodig has decreased on Guam over the last 50 years, other diseases like ALS, PD and Alzheimer’s have become more common. Steele is currently working with another neurologist, Douglas Galasko, and other researchers to pursue further the connection of lytico-bodig to unique environmental factors or some genetic link. This could be deduced from the observation that in families with multiple sick individuals, younger members seem to suffer from ALS, older members with PD and the eldest members with Alzheimer’s.
There have also been cases of non-Chamorros getting the disease after moving to Guam, and cases of Chamorros getting the disease who had never lived on Guam. These findings suggest both an environmental and genetic connection to lytico-bodig, however, in the coming years, new research focusing on disease transmission caused by an infection of abnormal proteins in the nervous system will likely emerge.
Seasonality and infectious disease
In a presentation at the Marianas History Conference held on Guam in 2013, biomedical researchers Vince Diego (TBRI) and Frank Camacho (from the University of Guam) discussed another approach to understanding the cause of ALS-PDC: seasonality and infectious disease. In 1972 Gibbs and DC Gajdusek hypothesized that ALS-PDC showed a “seasonality in incidence,” or was related to some kind of seasonal pattern or environmental change that occurred, causing an increase in the number of afflicted individuals. This idea was also supported by Jane Underwood in her demographic research on the disease.
The mosquito-borne Japanese encephalitis virus (JEV) was suggested as an agent that caused ALS-PDC. However, the seasonality of ALS-PDC also coincided with other hypotheses, including the metal hypothesis and the cyanobacterial toxin hypothesis. Diego and Camacho proposed that perhaps poliomyelitis would be a better candidate as an infectious agent because it coincides not only with seasonality, but also with historical events that occurred on Guam and Rota.
In situations involving what has been called “antecedent poliomyelitis,” the polio virus, which is water-borne, was contracted early in life and was shown to cause ALS, PD and Alzheimer’s later in life. That is, there is in these cases an established etiologic link between bouts of encephalitic infection early in life with neurological disorders later (often much later) in life.
Several historical resources report an epidemic of poliomyelitis that occurred in the late 1800s to early 1900s that coincides with the age of exposure to the polio virus and the age of onset of ALS-PDC for individuals later in life. In 1899, a steamer arrived from Manila and a poliomyelitis epidemic broke out shortly afterward. In the same year, the same epidemic was observed in the northern islands, including Rota, which may have been brought there by the same steamer or by infected individuals who traveled from Guam to the northern islands over the course of the epidemic. People from Malesso’ and Humåtak in particular were affected by the epidemic–the same villages that would show the highest incidence of lytico-bodig in the years that followed. Dr. William Hammon, who was widely considered to be among the top three poliomyelitis investigators in the United States (along with Jonas Salk and Albert Sabin), analyzed Guamanian serological data from the 1940s and interpreted these data to support the notion that polio was endemic to Guam since the 1899 epidemic.
Building from Underwood’s data and the historic records, Diego and Camacho propose a birth-month seasonality and secondary sex ratio to help explain the occurrence and pattern of lytico-bodig (ALS-PDC) on Guam. The polio virus generally infects very young children and JEV predominantly infects children between three and six years of age. Diego and Camacho suggest that children on Guam and Rota may have been affected by the polio virus, perhaps as newborns or shortly thereafter, and may also have been affected by JEV later between three and six years of age.
It is also possible that these infections occurred and then a combination of environmental factors–including cyanobacteria toxins or aluminum levels or fadang/cycad toxins–could have triggered the disease as seen later in life.
Still a mystery
The exact cause of lytico-bodig has eluded the scientific community for decades and likely will remain a mystery for years to come. At its peak after World War II, there were as many as 60 people suffering from the disease. When the disease was observed in the 1950s and formal study begun, it may have already been in decline.
Questions about who is susceptible to getting these neurodegenerative disease, whether through genetics, environment or a combination of both, are still to be answered. Scientists are pursuing the non-science study of history and society to determine if there were any record of significant events or contact with outsiders that could shed light on health and disease of these relatively isolated populations.
The story of lytico-bodig has largely focused on the medical or clinical aspects of the disease and rarely on the individuals who suffered from it, although Keck’s monograph, which included interviews with patients and their family members, represents a welcome remedy to this trend. The debilitating nature of lytico-bodig as well as the loss of life clearly has an impact on families, especially those families that have had more than one member with the disease.
Although lytico-bodig has recently mostly been seen in older patients, some individuals got sick while relatively young, leaving behind devastated children and relatives. There was not only the sadness of losing loved ones and moving on, but also the fear that one was susceptible to the disease and might get sick, too.
Guam’s unique history of colonization, population changes and cultural practices may have had an impact on the way diseases like lytico-bodig may have been observed to run their course. Perhaps historical epidemics, typhoons or some occurrence of depopulation resulted in a people genetically more susceptible to lytico-bodig. The areas of Guam with the highest occurrence of the disease have similar environmental conditions and lifestyles.
As the disease disappears with the passing of time, it remains a unique feature of Guam and the Chamorro people who have borne the pain of the disease itself and the scientific collection of data and information in the hopes of bringing greater understanding of this and possibly other neurodegenerative diseases in the world.
Editor’s note: Guampedia thanks Dr. Vince Diego for his kind assistance in completing this entry.
For further reading
Aoki, Dance. “Local Mystery May be Key to Curing Other Diseases.” Pacific Daily News, 10 October 2013.
Diego, Vince P., and Frank A. Camacho. “Birth-Month Seasonality and Secondary Sex Ratio in Guamanian Amyotrophic Lateral Sclerosis and Parkinsonism-Dementia Complex: Implications for Infectious Disease and Environmental Etiologie.” Paper presented at the 2nd Marianas History Conference, University of Guam, 29 August 2013.
Garruto, Ralph M., and Richard Yanagihara. “Contributions of Isolated Pacific Populations to Understanding Neurodegenerative Disease.” Folia Neuropathol 47, no. 2 (2009): 149-170.
Keck, Verena. The Search for a Cause: An Anthropological Perspective on a Neurological Disease in Guam, Western Pacific. Mangilao: MARC Publications, University of Guam, 2011.
Plato, Chris C., Ralph M. Garruto, Douglas Galasko, Ulla-Katrina Craig, Meropi Plato, Anthony Gamst, Jose M. Torres, and Wigbert Wiederholt. “Amyotrophic Lateral Sclerosis and Parkinsonism-Dementia Complex of Guam: Changing Incidence Rates during the Past 60 Years.” American Journal of Epidemiology 157, no. 2 (2003): 149-157.
Steele, John C., and Patrick L. McGeer. “The ALS/PDC Syndrome of Guam and the Cycad Hypothesis.” Neurology 70, no. 21 (2008): 1984-1990.