Guam Pattera (Nurse Midwives)
Editor’s note: The following was adapted from The Pattera of Guam: Their Story and Legacy written by Karen A. Fury Cruz which was made possible, in part, from the Guam Humanities Council in cooperation with the National Endowment for the Humanities.
Nurse-midwives
The CHamoru women who were trained as nurse-midwives by the US Navy assisted with home births in Guam from approximately 1910 to 1967. CHamorus born on the island during this period were most likely to have been delivered by one of these nurse-midwives. These women, known in Guam as pattera, play a unique role in Guam’s history and culture.
The title pattera derives from the Spanish word partera, which means midwife. Old and Middle English define midwife as “with woman” and designates a woman who assists other women in childbirth. In former times and around the world, women have attended and assisted other women during labor and birth. In Guam, lay midwives and suruhåna, female CHamoru herbal doctors, assisted women during labor and birth.
The pattera served as the link between the CHamoru traditions surrounding childbirth and US hospital-based birthing practices. Furthermore, they embodied those times of change when Guam experienced the transition from the era of US Navy administration to self-government and, in the 1940s, survived the ravages of World War II. They merged their roles as mothers and wives with a career. When appropriate, they applied both indigenous and US practices of health care and economics. And these women became Guam’s first CHamoru self-employed, licensed health practitioners.
Some nurse-midwives worked for the Division of Public Health and others for the hospital, but most worked independently in villages throughout the island. They traveled on foot or by bull cart and later by motorized vehicles to assist in home births. They were also trained to refer patients with abnormal or complicated pregnancies to a physician or to the hospital.
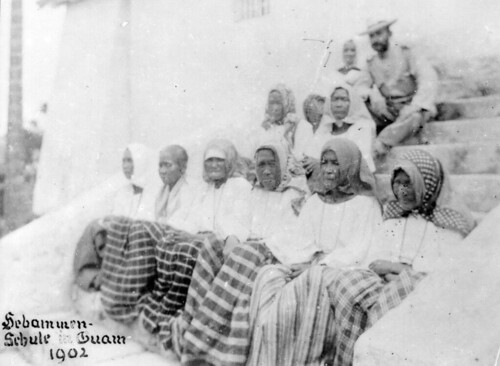
Training began in 1907
Training of nurses and nurse-midwives in Guam began in 1907 when US Navy medical officers established a school for their instruction and licensing. Previous to this, a governor’s order in 1900 instituted a course in elementary gynecology and antisepsis at the US Naval Hospital, a required course for the licensing of lay midwives. In 1910, the Naval Hospital Bureau of Medicine and Surgery recruited three Navy nurses to organize what was called the Training School for Native Nurses. All graduates of the three-year training program were given a midwifery permit if they completed three months of postgraduate work in the hospital.
Student nurses had to be unmarried. They worked eight hours a day, with permission to go home one day a week, and received $9.92 per month. The training was conducted at the US Naval Hospital in Hagåtña, which was located where the Nieves Flores Memorial Library now stands. The hospital had three wards:
- Ward I, or the Maria Schroeder Hospital, that opened in 1901 to care for CHamoru males over 12 years of age and military male personnel;
- Ward II for enlisted men;
- Ward III, known as the Susana Hospital, for women and children.
It is likely that students from villages other than Hagåtña did not go home very often for lack of transportation. In 1922, the nurse-midwife training program was described as being a two-year program with fifteen students always in training. The training placed special emphasis on obstetrics. Graduates of the program were “examined and given midwife certificates for one year,” at which time recertification or relicensing was required.
The training for nurses and nurse-midwives in Guam was described as “loosely organized” until the early 1930s when a formal curriculum was structured. This date may seem surprisingly late, but nurse-midwifery was recognized as a health profession in the United States only in 1925, and it was not until 1931 that the Maternity Center Association of New York City established the first nurse-midwifery education program in the United States.
The formally organized three-year nursing course of classroom and lab instruction that existed in 1934 included nursing skills, dietetics, drugs, anatomy and physiology, hygiene and sanitation, bacteriology, ethics, medical, surgical, obstetrics, pediatrics, contagious diseases, operating techniques, and so forth. All graduates received a midwifery permit, if requested, and, as before, those practicing midwifery were required to have three months of post-graduate work in the hospital. The post-nursing training for midwifery is a concept similar to today’s various nurse specialist occupations, one of which is the certified nurse-midwife.
In 1941, World War II interrupted the nursing school operations. The last nurse to graduate had pin number 89. After the war, in October 1945, the US Navy reestablished the nurse training school. They modeled the curriculum after approved schools in the United States. An obstetrics and midwifery course was included in the third and final year of training.
The nursing school closed after the enactment of the Organic Act of 1950, which marked the beginning of civilian administration for Guam. The last class of the then-named Guam Memorial Hospital School of Nursing graduated in 1952. Thus, nurse-midwife training in Guam came to an end.
General or district licenses
Certification and licensing of health practitioners is a method of regulating and defining the practice and training requirements of practitioners. In the United States, three types of midwives are generally recognized: certified nurse-midwives, licensed or certified midwives, and lay midwives. Licensing of midwives was first established in Guam by the US Navy administration. A governor’s order on 1 November 1900 required all practicing midwives in Guam to be licensed; however, training and examination requirements had to be met before a license was issued.
Midwife licenses were issued, beginning in 1925, for one of two categories of practice, either for general or for district. These categories presumably defined geographic areas of practice, that is, islandwide versus a specific village. Because of the advent of nurse-midwife training, many of the practicing midwives were also trained nurses. According to a 1927 governor’s report, nurses who trained especially in maternity care were licensed as midwives. The enactment of the Nurse Practice Act in 1952 established only one class of midwife license and administratively separated the licensing of nurses and midwives.
Number of Nurse-Midwives uncertain
The number of nurse-midwives trained and licensed was not always reported. From 1918 to 1921, there were 13 to 18 midwives licensed annually; 46 midwives were licensed in 1928; and 47 in 1931. In 1937, 42 midwife licenses were issued: 38 for nurses, one for a graduate of the training school, and three for lay women, all of whom were issued a district license.
After World War II, there was a decrease in the number of licensed midwives. In 1946, 21 midwives were licensed, a 50 percent decrease compared with prewar (1937) numbers. By 1949 the number of licensed nurse-midwives had increased to 28. The increase is presumably due to the reestablishment of the training program after the war.
Compensation allowed
Midwives in indigenous societies, as well as in rural American and European communities, typically received a gift for delivering a baby. This, according to the literature, distinguishes midwifery from traditional healers, who believed acceptance of a payment reduced their healing powers. In Guam, public law determined midwife fees and payment practices. In 1925, a fee of $2.50 to $10 per patient was allowed to be paid to the attending midwife upon discharge of the patient. Patients could stay at the hospital at no cost. Persons living in Hagåtña had to request that the hospital assign them a midwife. The midwife had the right to decline a case if nonpayment was anticipated.
In 1936, an amended law guaranteed midwives the right to a $10 fee. In 1952, the fee was increased to a $25 minimum.
In actuality, pattera often performed their services without receiving any cash payment. They would never decline a request for help even though the law permitted them to do so on presumption on nonpayment. To refuse service would have been legal, but not culturally appropriate. Families unable to pay in cash showed their gratitude to the midwives by giving them produce from their ranch or garden.
Improved health care
From the early 1900s, the government reported the number of deaths and births in Guam. This was one way to determine an increase in the population, which would indicate improved well-being and good health among the population. Official reports focused on sanitation, leprosy and other infectious diseases, and medical care through dispensaries and the hospital.
The US Navy provided instruction for lay midwives in 1900. Governor Seaton Schroeder ordered instruction in sanitary methods by the Navy medical officer for all lay midwives. Training of nurse-midwives was one of the US Navy’s planned measures for improving the health of Guam’s population. The overall effects of the health care program in the first four decades of the century contributed to a 120 percent increase in population and a drop in the death rate from 29/1,000 in 1905 to 13.9/1,000 in 1940.
During the Japanese occupation of Guam, from December 1941 through July 1944, the nurse-midwives continued to attend births, performing midwifery, first aid, and provide general nursing services. Their services were critical in this time of need because other health care services, which had been largely dependent on US Navy personnel, were interrupted by war.
In the 1950s, public health services available to the people of Guam included a nurse-midwife who held biweekly prenatal clinics in each district and who was able to see nearly all the pregnant women who were unable to afford private doctors or were ineligible for Naval hospital care. Pregnant women who chose to deliver at the civilian hospital received prenatal care at the central clinic.
The self-employed nurse-midwives continued to assist those women who chose to deliver their babies at home. The Public Health Division reported that the “midwives of Guam have a creditable record” and that the record “speaks well for the judgment and conscientiousness of the midwives.” “There [was] no report of infection following home deliveries.”
The pattera legacy
Tinifok Estoria Siha: Their Stories Woven Together
Each pattera has a unique story to tell. By bringing their stories together, commonalities emerge that go beyond the shared experiences of training, practice protocols, and licensing requirements. The commonalities are instead like the fibers of the tåli (rope), which when brought together give substance, form, function and value. The following commonalities can be seen as fibers that tie together the past with the present and define the pattera legacy to Guam.
- The pattera were present to assist mothers in childbirth, give support to the family during this most significant event, and assure the well-being of both mother and child. The pattera gave witness to the birth of thousands of babies, Guam’s future generations. Their reports became the official records of birth.
- Women and men, either relatives or acquaintances, and others, played a key role in the careers of the pattera. They prompted and encouraged these women to enter nurse training and to pursue and continue their work as midwives. Older CHamoru nurses served as role models and mentors.
- The opportunity to learn and to earn money for themselves and their families held significant importance. Some nurse-midwives did not have the benefit of much formal education prior to entering nurse training. For most CHamorus of school age in prewar Guam, only an elementary school education was available. Before World War II, the Naval government viewed a high school education as “unnecessary except for a few,” and separate schools beyond the sixth grade provided practical training in homemaking and agriculture.
- The motivation for pattera that prevailed over time was the desire to help others. They dedicated themselves to this. The timing of a birth is not something that is scheduled at one’s convenience, so the pattera availed themselves any time, day or night. Pattera faced difficulties in getting transportation to various locations, but this was not a barrier to reaching the women who needed their help.
- The self-employed pattera was an independent and trusted practitioner. The pattera worked in people’s homes outside of institutional settings and without direct supervision. Some CHamoru people critically viewed the independence of the pattera and their working relationship with American men (US Navy personnel), but nonetheless, the women persevered. Their attitudes and behavior reflected independent thinking and self-confidence while maintaining a respect for others and legal authority.
- The extended family provided immeasurable support to the pattera by caring for the children and home when the women were away assisting with a birth. A few nurse-midwives also provided services in their own homes. Such arrangements made managing the combined roles of wife, mother and pattera much easier for the women.
- For many pattera, their families and abiding faith in God provided a supportive foundation that sustained them over the years. It was to their families and their God that they gave credit and from whom they drew strength.
- The pattera took pride in their work and, though unspoken and unsolicited, pride in themselves.
By Karen A. Fury Cruz, RN, MPH
Film
For further reading
DeLisle, Christine Taitano. “Delivering the Body: Narratives of Family, Childbirth and Prewar Pattera.” MA thesis, University of Guam, 2000.
–––. Placental Politics: CHamoru Women, White Womanhood, and Indignity under US Colonialism in Guam. Chapel Hill: University of North Carolina Press, 2022.
Guerrero, Oliva. “Growth of Nursing on Guam.” Pacific Profile 3, no. 4 (May 1965): 14-15, 41, 43-44.
Guevara, Claudia. “I Pattera.” Glimpses of Guam 15, no. 3 (1975): 60-63.
Haddock, Robert L. A History of Health on Guam. Hagåtña: Cruz Publications, 1973.
Hattori, Anne Perez. Colonial Dis-ease: U.S. Navy Health Policies and the Chamorros of Guam, 1898-1941. Pacific Islands Monograph Series 19. Honolulu: University of Hawai`i Press, 2004.
–––. “‘The Cry of the Little People of Guam’: American Colonialism, Medical Philanthropy, and the Susana Hospital for Chamorro Women, 1898-1941.” Health and History 8, no. 1 (2006): 4-26.
I Manfåyi: Who’s Who in Chamorro History. Vol. 1. The Hale’-ta Series. Hagåtña: Political Status Education and Coordinating Commission, 1995.
“The Native Nurse Corps.” Guam Recorder 14, no. 6 (1937): 27, 42.
US Navy Department. Information on Guam Transmitted by the United States to the Secretary-General of the United Nations. OPNAV-P22-100G. Washington, DC: OPNAV, 1949.
Workman, Ann M., Linda Cruz Ortiz, and Debbie Kaminga-Quinata. “The Use of Traditional Medicine and Healers on Guam” In Science of Pacific Island Peoples: Fuana, Flora, Food and Medicine. Vol. 3. Edited by John Morrison, Paul Geraghty, and Linda Crowl. Suva: Institute of Pacific Studies, University of the South Pacific, 1994.